The macula, scientifically referred to as the ‘macula lutea’ or ‘yellow spot’ in Turkish, occupies the central region of the retina. This intricate part of the eye plays a pivotal role in providing us with both clear and colorful vision, essentially serving as the linchpin for our central vision.
In the following article, I will delve into the topic of macular holes, exploring the reasons behind their occurrence in the visual center, elucidating their symptoms, detailing the diagnostic process, and shedding light on various treatment options. Additionally, I will touch upon the success rates associated with surgical interventions for this condition.
What is a Macular Hole?
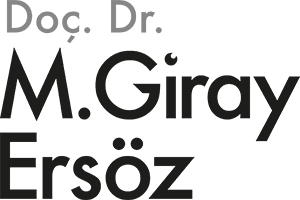
As a consequence of the separation of cells within the macula, our central visual hub, a circular void emerges amidst the visual cells. This particular void within the macula is medically termed a ‘macular hole,’ often colloquially referred to as a ‘hole in the point of vision’ or a ‘hole in the yellow spot’ due to its location. This nomenclature can sometimes lead to confusion, as it is frequently mistaken for age-related macular degeneration. It is essential to note, however, that macular hole and age-related macular degeneration are distinct and separate medical conditions, each with its own unique characteristics.
Why Do Holes Occur in Our Visual Center?
Macular holes typically manifest spontaneously, often initiated by the gradual separation of the vitreous gel from the retina at the back of the eye. As this separation progresses, it can lead to the contraction and formation of holes in the delicate macular region. It’s worth noting that individuals who experience a spontaneous macular hole in one eye are at an elevated risk of developing a similar condition in their other eye. In rarer instances, macular holes may also develop as a result of eye trauma or among individuals with high degrees of myopia.
What are the Symptoms?
In one eye, macular hole disease typically starts subtly. Therefore, we perceive the objects as slightly bent or distorted when we look with the eye, which begins to form a hole in the first stage. The visual center is severely impacted as the hole widens over the course of weeks and months, and as a result, our ability to drive and read is hampered.
Reduced and blurred vision, difficulty reading, broken vision, and the inability to see the center of an object are all possible symptoms of a macular hole. Patients with macular hole experience changes in the center of their vision. In stage 1, these modifications take the form of breaking and bending in straight lines, whereas in stage 2, they manifest as seeing a fixed blind spot in the visual center. From stage 2 to stage 4, the macular hole gradually gets bigger. As the macular hole widens, the area of impaired central vision expands, leading to a gradual decline in overall visual acuity. It’s important to note that complete blindness resulting from macular hole disease typically only occurs when it is concurrent with retinal detachment. However, when left untreated for an extended duration, a macular hole can ultimately result in the complete loss of central vision. This often leads to a significant reduction in visual capability, falling below the legal threshold for blindness, typically within the range of 2-5%.
Who is Prone to Macular Hole?
Macular hole is generally seen after the age of 50. This disease often occurs in women, and when the statistical data of macular hole cases are examined, it is seen that women constitute two-thirds of them.
How is a Macular Hole Diagnosed?
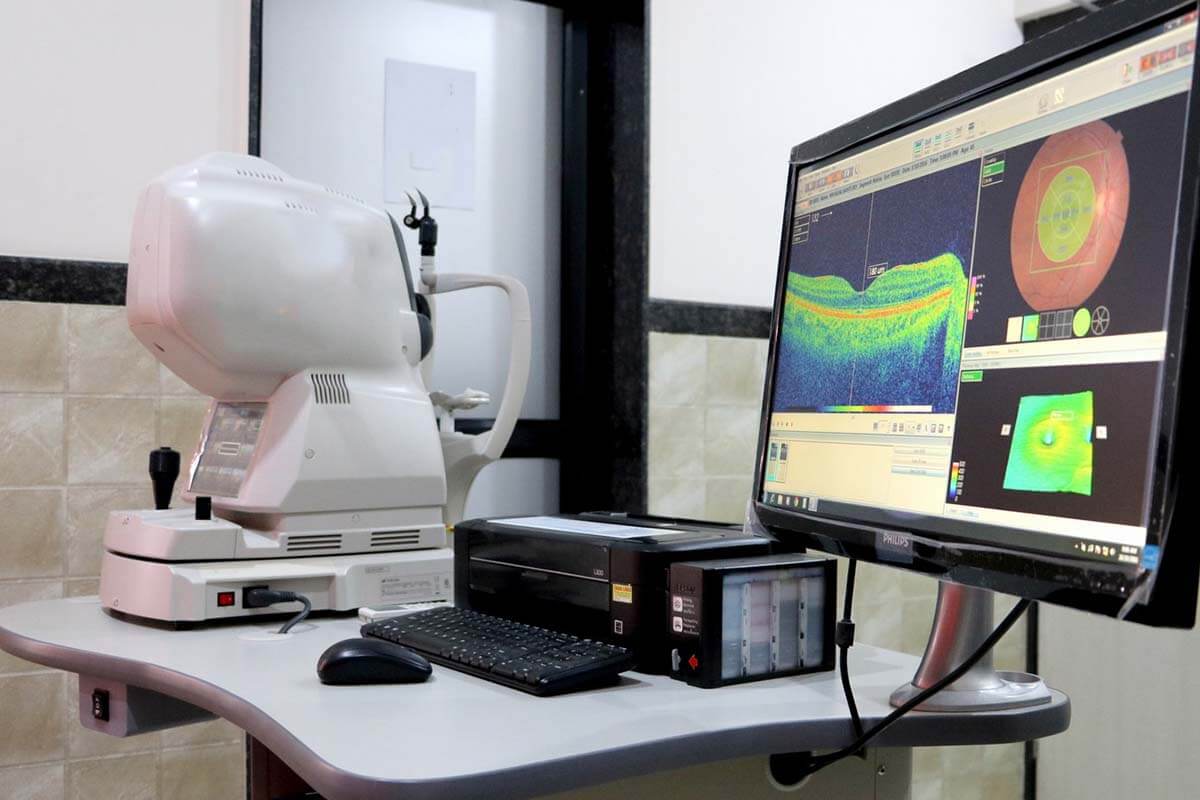
Following a routine eye exam, a posterior eye with eye drops (bottom of the eye) examination is carried out to help identify a macular hole. Patients with suspicions of a macular hole undergo optical coherence tomography (OCT or OCT), also known as eye tomography, which uses light waves to visualize the retina and has no negative side effects. The other eye’s vitreomacular interface and outer retinal layers can also be thoroughly examined with OCT to assess the risk of macular hole formation in addition to making the diagnosis.
What are the Macular Hole Stages?
Depending on the size and duration of the macular hole, there are four different stages. The size of this gap in our visual center keeps expanding, and so does its phase. Vision gets worse as the macular hole progresses. The smallest macular hole is a stage 1 macular hole. The largest and most severe macular holes are referred to as stage 4 macular holes. Let’s now take a closer look at the macular hole’s stages;
Stage 1
The macular hole’s potential location is initially flattened, and the symptoms are essentially nonexistent. There is a chance that the macular hole will heal on its own if treatment is delayed at this point.
Stage 2
The macular hole has manifested and the symptoms are clear in stage 2. Weak vision or the perception of dark spots are signs of central vision problems. The surgical intervention to close the hole is tense at this point, but the likelihood of success is very high.
Stage 3
At this point, the macular hole has grown even larger, the retina’s connection to the vitreous fluid has been totally severed, and our central vision has been significantly compromised.
Stage 4
The macular hole has now grown significantly and is in its final stages. It is a sign that a lot of time has passed since the disease first manifested itself. The macular hole still has a chance to be treated at this point.
How to Treat Macular Hole?
The only available treatment for the macular hole is vitrectomy surgery; medication cannot be used to treat it. Anesthesia options for the procedure include local or general. Ophthalmologists who have received additional training in retinal surgery perform vitrectomies.
The thin membranes in the macula region that cause shrinkage are peeled off during vitrectomy surgery, and then an air-like gas is injected into the eye.
In vitrectomy surgery, the procedure involves several key steps. Initially, the vitreous fluid within the eye is meticulously cleaned. Subsequently, delicate membranes that may contribute to the development of irregularities in the macula area are gently peeled away. The surgery is then concluded by introducing a gas with properties similar to air into the eye.
Following the operation, patients are instructed to maintain a continuous face-down position for a period of five days. This specific posture is crucial for the successful recovery and healing process. Additionally, patients are advised against air travel or visiting high-altitude locations until the gas within the eye naturally dissipates. This caution is important because changes in air pressure can lead to the expansion of the gas within the eye, potentially elevating intraocular pressure and, in severe cases, causing vision impairment.
Injections of SF6 and C3F8 gases into the eye during surgery both spontaneously disappear after two and six weeks, respectively. Surgery for a macular hole typically lasts 50 to 60 minutes. This spans the duration of the surgical intervention, from beginning to end. Exams and preoperative preparations are not part of this time frame.
Innovations in Macular Hole Surgery
The most recent and widely adopted surgical approach for treating macular holes is known as the ‘ILM Flap’ technique, which stands for ‘Internal Limiting Membrane Flap.’ In conventional macular hole surgery, the ILM membrane is entirely removed from the periphery of the macula. However, with the ILM Flap technique, instead of complete removal, the membrane is delicately peeled off from one area and then meticulously folded over the macular hole. This innovative approach can be applied to all types of macular holes, but it has notably elevated the success rate, particularly in treating larger and more advanced stage 3 and 4 macular holes.
What is the Success Rate of Macular Hole Surgery?
The success rates for macular hole surgery are notably high, particularly in the case of Stage 1 and Stage 2 macular holes, where they approach nearly 100%. However, as the stage of the macular hole advances, the probability of achieving hole closure diminishes. For larger holes, special surgical techniques can be employed, involving the use of a membrane from the retina to cover the hole. This technique significantly enhances the likelihood of successfully closing the macular hole.
The postoperative visual outcome is closely tied to the patient’s preoperative visual status. Typically, patients can anticipate a visual acuity improvement of approximately 10-30% following surgery. It is crucial for patients with macular holes to understand that without surgical intervention, the risk of complete loss of central vision is imminent. Therefore, timely treatment is essential to preserve their visual function.
What Are Common Post-Macular Hole Surgery Complications?
A 3-5% chance of retinal detachment exists in patients who undergo vitrectomy (retinal surgery) due to a macular hole. In patients recovering from surgery, cataract formation or progression is a very common condition.
Macular Hole Surgery Price
Vitrectomy surgery is performed for the macular hole and gas is injected into the eye. The price of macular hole surgery varies according to the technique to be used, the type of gas and the type of anesthesia.
What is RPE Change in the Macula?
The retinal pigment epithelium (RPE) cells are home to the retinal cells that allow us to see in the macula. The RPE cells at the bottom of the macular hole are exposed and start to suffer damage as soon as the hole forms. The beginning of RPE changes at the hole’s bottom shows that the hole has been patiently waiting for a while. The extent of the postoperative visual recovery will be lessened if there has been significant pigmentation in the RPE cells.
What Can Help With Macular Hole?
No amount of diet, vitamin supplementation, or exercise will cause the macular hole to heal on its own without surgery. Minor eye traumas can cause a macular hole in patients who are at risk for the condition. Therefore, it is suggested that these patients avoid participating in contact sports.
My Scientific Studies on Macular Hole
- First-Operated and Fellow Eyes With Bilateral Idiopathic Macular Hole: Comparison of Anatomical and Functional Postoperative Outcomes.
42 patients who first experienced a macular hole in one eye and then the other were included in this study, which was written up in the American journal “Ophthalmic Surgery Lasers Imaging Retina”. The results of our study show that even though the anatomical holes were successfully closed in both eyes, the second eyes’ visual acuities were statistically higher than the first eyes’. The cause of this is that when a hole develops in the second eye, patients seek medical attention more quickly.
- Double Arcuate Relaxing Retinotomy for a Large Macular Hole
It is demonstrated in this article from the journal “Retinal Cases Brief Rep” that in a patient with a very large macular hole, bilateral incisions made in the retina ensure the hole will close.
- Outcomes of Vitrectomy Under Air for Idiopathic Macular Hole
In this study, which was published in the Turkish Journal of Ophthalmology, 21 patients with macular holes underwent sub-liquid vitrectomy using the traditional technique and 21 patients underwent under-air vitrectomy, a novel technique. The group that underwent vitrectomy under air experienced a statistically significant reduction in the length of the procedure. Both groups achieved 100% anatomical success, and there was no difference in retinal sensitivity between the two groups. According to the findings of our study, vitrectomy under air offers a benefit in macular hole surgery because it offers a larger field of vision and cuts down on operating time.
- When Does Visual Acuity Stabilize After Macular Hole Surgery? Five-year follow-up of Surgery for Idiopathic Macular Hole
We looked at 162 eyes of 146 macular hole patients in this study, which was published in the UK journal “Acta Ophthalmologica” with a 5-year follow-up. We discovered that the improvement in visual acuity in these eyes increased statistically significantly over the course of two years and then stabilized.
- Characteristics and management of macular hole developing after rhegmatogenous retinal detachment repair.
In this study, 1661 eyes that had undergone retinal detachment surgery were examined, and it was found that 14 of them had developed macular holes. The study was published in the Japanese Journal of Ophthalmology. The study also included patients who were referred to our clinic from 9 other eye-care center, and 23 cases of macular holes after detachment surgery were assessed. The macular holes that developed after detachment surgery were more complex, but the patients in our study had statistically significant improvements in visual acuity after the procedure.