Macular degeneration stands out as a prevalent factor contributing to vision loss, commonly recognized under the name age-related macular degeneration (AMD). This condition typically surfaces in older individuals, leading to progressive vision impairment. In this article, we will delve into the intricacies of macular degeneration, exploring its nuances, symptoms, diagnostic processes, and various methods of treatment.
What is Macular Disease?
The Macula, often referred to as the “Yellow Spot,” constitutes the central and vital region of the retina responsible for clear and central vision. It is an inherent structure present in all healthy individuals, enabling us to perceive the world with clarity. The term “macular degeneration” or “age-related macular degeneration” describes the deterioration that occurs in the macular area due to the natural aging process. In essence, this condition denotes changes in the macula, impacting its functionality and often affecting clear vision.

What are the Types of Age-Related Macular Degeneration?
Age-related macular degeneration is categorized into two primary types: Dry Macular Degeneration and Wet Macular Degeneration.
Dry Type Macular Degeneration:
Approximately 90% of age-related macular degeneration cases are attributed to the dry type. This classification arises from the absence of fluid accumulation, signifying damage to the cells within the macula, commonly known as the yellow spot. In the initial phases of dry type macular degeneration, lipid (fat) deposits, referred to as drusen, begin to accumulate beneath the retina. The genesis of these deposits is linked to the diminished capacity of retinal pigment epithelial cells to clear them with the aging process. Over time, cells in the drusen-affected area undergo degeneration. In the advanced stages of the disease, extensive areas of damage, termed geographic atrophy, emerge. Individuals with geographic atrophy experience impaired vision in specific areas of their central visual field, contingent upon the extent of the damage.
Wet Type Macular Degeneration:
The alternative form of macular degeneration is termed the wet type, distinguished by the presence of fluid accumulation in the macula. Accounting for 10% of macular degeneration cases, wet macular degeneration involves the development of new vessels within the choroid layer beneath the retina, responsible for nourishing the macula. However, these vessels form irregularly, leading to the leakage of fluid beneath and into the macula. Without intervention, the progression of the disease may result in bleeding from these vessels, further exacerbating the condition both within and under the macula.
Classification of New Vessels in Wet Macular Degeneration:
The assessment of new vessels in wet macular degeneration involves a threefold categorization. In Type 1 wet macular degeneration, the emerging vessels are situated beneath the retinal pigment epithelium. Progressing to Type 2, these new vessels penetrate the retinal pigment epithelium and extend into the retina. Type 3 wet macular degeneration, marks the onset of new vessel development directly within the retina. This nuanced classification helps in understanding the varying presentations of wet macular degeneration, aiding in tailored approaches to diagnosis and treatment.
Causes of Macular Degeneration:
As the name implies, the primary cause of age-related macular degeneration is the natural process of aging. This condition is believed to result from the premature aging of cells within the macula. While macular degeneration is observed in 0.2% of the population aged 55-64, its prevalence rises significantly to 13% among individuals over 85 years old. Additionally, certain risk factors beyond aging may contribute to the onset of macular degeneration.
Risk Factors for Macular Degeneration:
The prevalence of macular degeneration is notably higher in European societies compared to Africans and Asians, with a twofold increased occurrence. Smoking emerges as a significant risk factor, doubling the likelihood of macular degeneration and delaying its onset by approximately a decade.
A familial history of macular degeneration is another noteworthy risk factor, indicating a genetic predisposition to the condition.
In addition to these factors, proven contributors to an elevated risk of macular degeneration include prolonged exposure to sunlight, high cholesterol levels, hypertension, and heart diseases. Recognizing and addressing these risk factors are crucial steps in proactive management and preventive measures against the onset of macular degeneration.
Symptoms of Macular Degeneration (Age-Related Macular Degeneration):
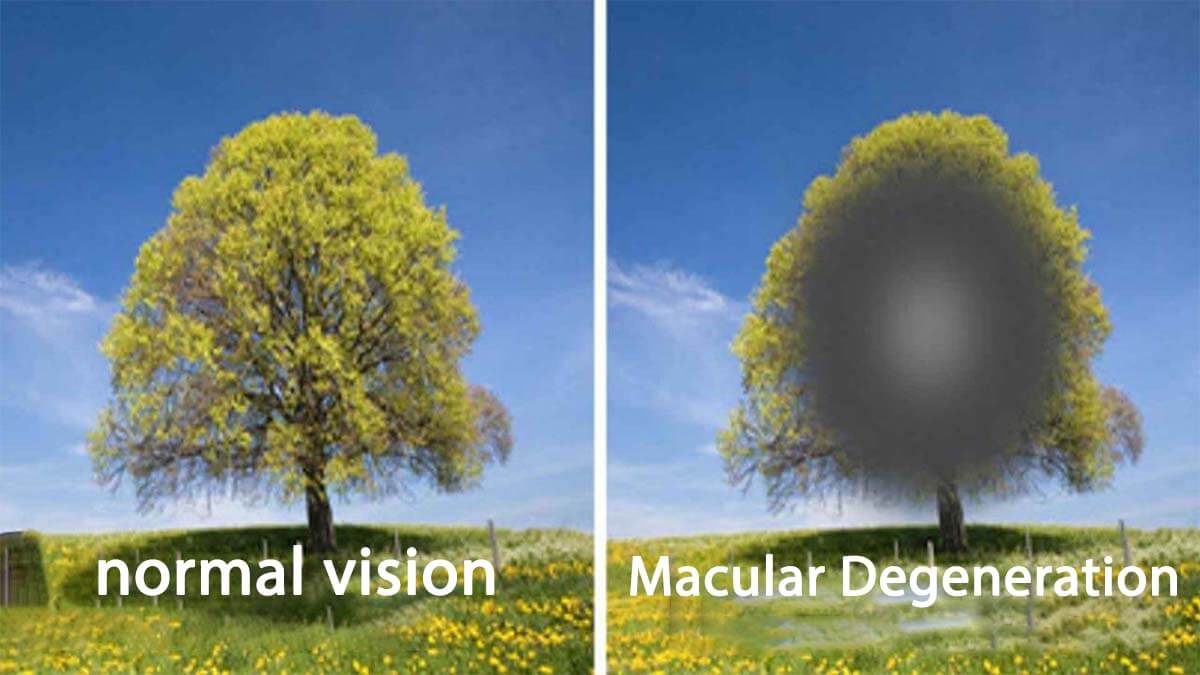
In its early stages, macular degeneration may not manifest noticeable symptoms. However, as the disease advances, various indicators emerge, including diminished vision, distorted or oblique vision, visual disruptions, difficulty in reading, and eventual loss of central vision.
Without intervention, the progression of macular degeneration can lead to a complete loss of central vision, leaving individuals with the ability to perceive only from the peripheral edges. Recognizing these symptoms early on is essential for timely diagnosis and the implementation of appropriate treatments to mitigate vision loss.
Diagnosis of Macular Disease:
Macular degeneration is diagnosed through a comprehensive examination involving eye tomography (OCT), color fundus photography, and fundus autofluorescence imaging conducted after a thorough eye drop-assisted examination. For a more precise diagnosis and differentiation from other age-related conditions, fluorescein angiography or indocyanine green angiography may be necessary. Individuals at risk can also perform self-screening using the Amsler grid test.
Given that macular degeneration may not initially present symptoms, it is advisable for individuals aged 55 and above to undergo regular eye examinations. These examinations play a crucial role in early detection and prompt intervention.
Conditions Confused with Macular Degeneration:
As the term “macular degeneration” refers to the macula, the central point enabling central vision, various diseases affecting the macula can be mistaken for age-related macular degeneration. These conditions include macular hole (macular hole), epiretinal membrane (ERM, membrane growth in the yellow spot), diabetic macular edema (edema related to diabetes), retinal vein occlusion-induced macular edema, and central serous retinopathy (CSR).
For a detailed understanding of macular hole disease, refer to “What is Macular Hole?” In-depth information on epiretinal membrane disease symptoms can be found in my article “Epiretinal Membrane Symptoms,” and for insights into central serous retinopathy, please refer to “Central Serous Retinopathy Symptoms.” These resources provide answers to specific questions related to these conditions often confused with macular degeneration.
Treatment for Macular Disease:
Halting the progression of dry macular degeneration remains elusive; however, vitamin supplements, known as micronutrition, are administered to mitigate the advancement of the disease. In cases of the wet type, intraocular injections are employed to regress the growth of abnormal vessels, effectively draining fluid and alleviating bleeding from the macula.
Vitamin Therapy:
Micronutrition refers to vitamin and mineral supplements aimed at slowing down the progression of dry macular degeneration. The AREDS-2 study substantiated the efficacy of micronutrition pills containing vitamin C, vitamin E, zinc, copper, lutein, and zeaxanthin in managing dry age-related macular degeneration. While omega-3 supplements like DHA and EPA, along with beta-carotene, were initially recommended in the AREDS study, beta-carotene was later excluded from these supplements. Some micronutrition pills still contain omega-3 components. Recent reports also suggest the potential effectiveness of supplements such as astaxanthin, resveratrol, and saffron in slowing down the progression of macular degeneration.
Intraocular Needle Injections:
To address the development of new and damaged vessels in wet macular degeneration, intravitreal injections from the anti-VEGF group are administered directly into the eye. These injections aim to regress the growth of abnormal vessels, facilitating the removal of fluid and blood from the macula. It’s crucial to note that while these injections effectively target and regress the branches of damaged vessels, they do not impact the main vessels. Consequently, new branches may emerge from the main vein over time, necessitating the need for subsequent injections.
Patient responses to intraocular injections can vary, prompting the adoption of individualized protocols. In the personalized intraocular injection protocol introduced by Assoc. Prof. M. Giray Ersöz, three injections are administered one month apart initially. Subsequent intervals are then adjusted based on the patient’s response to these initial injections. If there is minimal or no fluid present, treatment intervals are extended by two weeks, while recurring intense fluid may lead to a reduction in treatment intervals. The ultimate goal is to prolong treatment intervals to three to four months.
For instance, if, after three injections given four weeks apart, no fluid remains in the macula, the subsequent injection is administered six weeks later. If the patient returns after six weeks with minimal or no fluid, the subsequent injection occurs after eight weeks. Should fluid be present, and vision remains stable after eight weeks, the following injection is again scheduled for eight weeks. Conversely, if there is a significant fluid buildup and a decline in vision, the subsequent injection is administered after six weeks. This patient-specific approach strives to establish a tailored treatment protocol, maximizing the interval between injections to achieve the longest possible duration without compromising vision.
It’s important to highlight that intraocular anti-VEGF injections are not effective in treating dry-type macular degeneration.
Intraocular Injection Procedure and Post-Procedure Care:
Intraocular injections can be conducted in outpatient clinics or sterile environments within operating rooms. Assoc. Dr. M. Giray Ersöz, for instance, performs these injections in dedicated sterile rooms within the polyclinic setting. The process initiates with an assessment of the patient’s vision on the day of the injection, followed by the application of eye drops to induce pupil dilation. Once the pupil is dilated, eye tomography (OCT) is performed to evaluate the presence of fluid in the macula, influencing the determination of the next injection date. Subsequently, the patient is ushered into the injection room, where their eyes and face are meticulously sterilized and covered with a sterile drape before the intraocular injection is administered.
After a brief rest period of 2-3 minutes, during which the patient’s eyes remain closed, they are discharged and advised to continue resting at home. The eye is to remain closed for the first day, only being opened for the application of prescribed eye drops. A five-day course of eye drops is typically recommended. While experiencing symptoms such as stinging, burning, or mild discomfort in the eyes on the day of the injection is normal, any severe pain or significant vision loss within the first two days post-injection warrants immediate consultation with an ophthalmologist.
Macular Disease (Amsler Grid) Test:
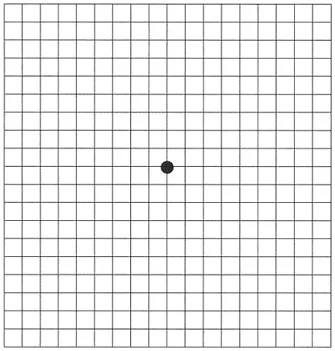
Testing Procedure:
Wear your glasses, if applicable.
Close one eye and focus on the central point within the gridded test from a distance of 40-45 cm.
Observe for any areas that you cannot see clearly or if you perceive distorted or uneven lines.
If abnormalities are detected, seek immediate consultation with an ophthalmologist.
Note: Repeat the same steps for the other eye.
Regular self-administration of the Amsler Grid test provides a simple yet effective means of monitoring your vision and promptly identifying any potential issues related to macular disease.
Frequently Asked Questions About Macular Disease:
- What Vitamins and Minerals are Beneficial for Macular Disease?
Vitamins C and E, zinc, copper, lutein, zeaxanthin, astaxanthin, resveratrol, and Omega-3 contents are particularly effective in slowing down the progression of dry-type macular degeneration.
- Which Foods are Recommended for Macular Degeneration?
A Mediterranean-style diet, emphasizing green vegetables and olive oil, is recommended for individuals with macular degeneration. Additionally, incorporating purple grapes, blueberries, blackberries, strawberries, and cranberries into the diet is beneficial due to their saffron and resveratrol content.
- How Does Macular Disease Occur in Babies and Children?
Macular degeneration is not observed in infants or children. However, some genetically inherited diseases impacting the macula may be present. Among these, Stargardt disease, cone dystrophy, and best disease are the most common.
My Scientific Studies on Macular Degeneration (Yellow spot disease)
You can find my scientific studies on macular degeneration below:
- Membrane Patterns in Eyes with Choroidal Neovascularization on Optical Coherence Tomography Angiography. doi: 10.1038/s41433-019-0415-1
Our research, featured in the esteemed ophthalmology journal, Eye, and published in England, delves into the analysis of 184 eyes from 153 patients afflicted with macular degeneration. The study outcomes revealed a noteworthy observation: the morphological characteristics of new vessels on optical coherence tomography angiography demonstrated no discernible association with clinical activity. However, a distinctive finding emerged, indicating that the presence of long dilated filamentous linear vessels was notably linked to chronicity and the state of lesion inactivity.
- Features of Neovascularization in Pachychoroid Neovasculopathy Compared with Type 1 Neovascular Age-Related Macular Degeneration on Optical Coherence Tomography Angiography. DOI: 10.1007/s10384-020-00730-7
Our research, now featured in the prestigious Japanese Journal of Ophthalmology, a highly regarded publication in the field, focused on 36 patients with type 1 neovascular age-related macular degeneration and 34 patients with pachychoroid neovasculopathy. Despite the younger age of patients with pachychoroid neovasculopathy compared to those with type 1 neovascular age-related macular degeneration, our study revealed a notable finding: no discernible difference in terms of new vascular patterns was observed between the two diseases in optical coherence tomography angiography.
- Risk-based Algorithm-guided Treatment Protocol for the Management of Neovascular Age-related Macular Degeneration. doi: 10.4274/tjo.galenos.2019.26235
Published in the Turkish Journal of Ophthalmology, our study encompassed 210 eyes from 184 patients diagnosed with age-related macular degeneration. The findings underscore a significant revelation: the implementation of risk-based individualized intraocular needle treatment proved effective in preserving vision levels, requiring fewer injections compared to conventional approaches.